What is Causing My Heel Pain?

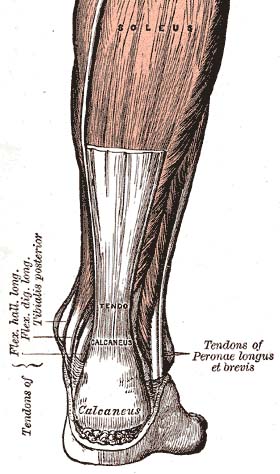
Image via Wikipedia
Heel pain can be caused by a number of factors. One of the most common is a heel spur, medically referred to as a calcaneal spur.
A heel spur is an outgrowth of bone in the shape of a small spire. If it’s at the bottom or side of the heel bone (calcaneous), it can be painful to walk. It is thought that heel spurs form as a result of stress on a tendinous insertion into to the heel, but some heel spurs aren’t associated with the area where a tendon inserts into the heel.
Whenever offshoots of bone form (bone spurs), it is due to a history of stress to the bone, either gradual formation following a single impact trauma such as a car accident; or cumulative impact forces over time, such as from sports. For the foot bones, an example of the latter would be years of playing basketball or ballet dancing. The repetitive pounding on the joints of the foot can cause bone cells at the impact area to secrete more bone matrix as a compensatory response. In the spine and large weight bearing joints (knee, hip) they are called osteophytes.
In some cases, the heel spur stops producing pain; perhaps due to resorbption or even callous formation neutralizing its ability to press against tissue. For those that don’t, surgery can be done by a podiatrist or orthopedic surgeon to smooth down the heel spur.
TREATMENT:
In the meantime, avoiding impact trauma to the heel is important (running, jumping). You can buy special shoe inserts that help reduce pressure on the heel spur. Comfortable shoes are a must as well; make sure they are wide and have a thick rubber, shock absorbing sole. The Z-Coil shoe brand incorporates a large spring at the heel to minimize shock/ impact forces to the foot when walking.
Sitting in a chair and rolling a cold beer or soda can (unopened) under your foot can help stretch the foot and ease some of the pain. A golf ball can provide more focused massage to the bottom of the foot. Press downward with enough pressure to get a good stretch and massage, but not so much to increase the heel pain.

Image via Wikipedia
Lastly, consider exercising your feet by walking barefoot around the house and outside (walking barefoot indoors is not as effective due to the flatness of the floor; bumpy and uneven is better). Walking in shoes actually weaken the foot over time by preventing the intrinsic foot muscles and joints from exercising and experiencing their full range of motion. You can also consider getting the Vibram foot glove. This interesting shoe fits on your foot like a glove, allowing some independent movement of the toes.
Plantar fascitis is a condition where the plantar fascia (a wide, band-like ligament connecting the heel to the forefoot) pulls off a thin layer of periosteum (membrane lining the bone) from the heel and results in inflammation and pain at the front, bottom part of the heel. It can make walking very uncomfortable.
The best approach to treating plantar fascitis is to rest your foot for a few days: no running, no walking up hill; walk only on flat surfaces. Use Red Light Therapy and Pulsed EMF for 15 minutes, twice a day for 2-3 weeks to accelerate healing of tissues, and for reducing any inflammation that is causing pain. Red light therapy uses photobiomodulation to accelerate cell metabolism; thus accelerating healing of tissues.
Compression fractures and hairline (stress) fractures can also cause heel pain. If you think you’ve fracture your heelbone, have it X-rayed. You’ll likely get a foot cast, avoid impact to the heel for several months, and wait until the fracture heals (no pun intended).