by Pain Doc | Aug 31, 2015 | Hand and Wrist Pain
Just like how sciatica/ leg pain is usually caused by a bulging disc in the lower back or by a muscle pinching the nerve, arm pain and/or numbness & tingling is usually caused by a bulging disc in the neck or by a muscle pinching a cervical (neck) nerve root or plexus.
The nerve roots that come out from between your cervical vertebrae converge to form three main nerves that service the arm: the ulnar, median and radial nerves. If any of these nerve roots are pressed by a bulging disc, a bone spur or thickened ligament, it usually causes radiating (traveling) pain from the neck down the arm; usually all the way down to the fingertips.
The specific area of pain/tingling depends on which nerve root is being pinched. In fact, that is how doctors diagnose the precise problem area. For example, numbness down the medial (inner) side of the forearm down to the pinkie and ring finger can be produced by compression of the C8 & T1 nerve roots. Numbness in the outer forearm, thumb and first two fingers is associated with the C6 & C7 nerve roots.

Radiating arm pain can also be caused by thoracic outlet syndrome, where muscles near the neck and upper shoulder pinch the nerve plexus (where the roots converge). This will be next week’s topic.
Self Treatment for Radiating Arm Pain
If you have significant neck pain accompanying your arm symptoms, then it is likely you have a bulging disc in your neck. It feels like a focused, sharp pain deep inside the neck on one side. Massage does not help this kind of pain.
Most mild to moderate cases of cervical disc bulges resolve with exercises and manual therapy. The severe cases usually require surgery to remove the disc portion that is pressing against the nerve. If you have a severe case, get a consultation from a spinal surgeon and a second opinion. If done in time, surgery can resolve the arm pain, but if the entire disc is removed the surgeon will fuse the vertebrae above and below the disc which will reduce your neck range of motion somewhat.
If the disc bulge or offending structure is allowed to compress the nerve root for an extended period it may result in permanent injury to the nerve. This means after surgically removing the bulge, you still may have numbness down the arm. This is why, for nerve compression conditions, time is of the essence.
Non-surgical candidates can do exercises to reduce the bulge size. For typical posterior bulges (bulges that protrude towards the back and one side of the vertebral body) try this: while standing, use your posterior neck muscles to pull your neck straight back, as far as you can; hold for 3 seconds. It may feel uncomfortable if your disc bulge is acute. Keep your chin tucked in so that the top of your head is level. Do eight times, twice a day for a couple of weeks; note changes in your neck pain and arm pain. Discontinue if it aggravates your condition. This movement gently presses the backs of the vertebral bodies together, which pumps the disc bulge back to center.
If the exercises help but you hit a plateau, try side bending your neck towards the side of the pain, very slowly; repeat six times. Again, note changes; discontinue if it aggravates the pain.
Recommended Lifestyle Changes
Forward bending of the neck and anterior weight bearing of the head (forward head posture) tends to make the cervical discs more vulnerable to bulging because in this position the vertebrae press the front part of the discs, pushing the jelly center (nucleus) towards the back.
Axial forces (straight down through the spine) to the neck can also make disc bulges worse. Any activity that involves jumping creates axial forces — running, basketball, gymnastics, mountain bike riding, sky diving, etc. It’s not a concern unless you do it frequently.
If you have a bulging disc in your neck with arm pain, here are some suggested lifestyle changes:
- Use a contoured neck pillow and sleep on your back.
- Work on improving your posture: eliminate forward head posture.
- Get a standing desk if your job requires a lot of sitting– it’s better for your back and neck.
- Use the Cervical PosturePump device to hydrate your cervical discs
- Strengthen your neck muscles so they offer more support to your neck.
- Avoid excessive jumping. If you like running, consider getting Z-coil or Gravity Defyer shoes (see below).
Treatment Accessories to Reduce Arm Pain from Disc Bulge
 PosturePump Disc Rehydrator
PosturePump Disc Rehydrator
This device uses specially designed air bladders, inflated by a hand pump to spread apart and extend neck vertebrae. This expands the discs, drawing in fluids and nutrients and also stretches the neck into its normal, ideal curvature.
 Anti-Shock Specialty Shoes
Anti-Shock Specialty Shoes
These specially designed shoes have powerful springs in the heel that significantly dampen the forces generated from running. Less shock to your feet, ankles, knees, hips, low back and neck.
 Vari-Desk Height Adjustable Portable Desk
Vari-Desk Height Adjustable Portable Desk
Place this lightweight desk on your traditional sit-down desk and switch its height between standing and sitting in less than five seconds. Choose to stand for as long as you like, then switch back– great for easing into standing while working, if you’ve been a desk sitter for many years.
by Pain Doc | Jun 12, 2014 | Uncategorized
–
–
It is estimated that at any given time, about 40% of the adult population experiences lower back pain. That means, today when you walk on a busy street full of pedestrians, four out of ten people you see are experiencing some degree of lower back pain. 50-85% of all people will experience lower back pain at some time in their lives.
–
For many cases of low back pain, the source of the pain emanates for the
intervertebral disc, or IVD. This is the fibro-cartilagenous material that connects vertebrae together and is responsible for bearing most of the weight placed on the spine. Its architecture is designed to absorb shocks using the incompressible nature of water (hydrostatic pressure), which is mostly contained in the nucleus pulposus of the disc. The nucleus serves to redistribute and dampen the forces placed on the spine so as to avoid damage. This comes in handy when walking, jumping, sitting, standing, and of course picking up heavy things.
–
Problems arise when the disc weakens, allowing internal derangements to occur. Basically this means shifts in the shape of the disc that alter the proper alignment and movement of the spinal joint segment, and/or block or partially block nerve pathways, causing nerve root impingement and pain down the leg.
–
One of the home care accessories I prescribe for my low back pain patients is the
PosturePump™ Spine Retrainer. This innovative device helps to rehydrate weak and bulging disc derangements by increasing the space between vertebrae using an air bladder controlled by a hand aspirator. As the disc volume increases, a negative pressure develops and a pressure gradient forms, which draws fluids (capillary blood), nutrients, oxygen and reparatory cells into the disc. This can help the disc regenerate, and the lumbar extension forced by the
PosturePump™ Spine Retrainer can mechanically force the posterior disc bulge back to center at the same time, relieving symptoms.
–
–
Even if you don’t have a bulging disc, the PosturePump™ can serve as a good preventive measure to keep your discs healthy and strong.
–
Watch the video to see how this works.
–
If you have recurrent pain of any type, stay tuned for further posts…you just might run into something that will make a significant impact on your quality of life. Please consider sharing this information, as it may be helpful to someone in your social circles. Thanks for reading!
–
Dr. Perez
by Pain Doc | May 25, 2011 | Uncategorized
 Inversion therapy tables are see-saw like contraptions designed to use gravity to decompress the spine. They have been around for more than twenty years already, so today’s models offer more in terms of comfort and ease of use. But the principle is the same: use a platform balanced on a horizontal rod, with a mechanism to offer some controlled resistance. You lie face up on the platform (more expensive models allow you to be face down), lock your feet into the foot carriage either by hooking your insteps onto rollers, or wearing gravity boots strapped to the carriage; and raise your arms in varying angles to control the amount of tilt. Arms extended straight above your head result in the maximum angle, usually around 45 degrees. The weight of your torso pulls gently on your spine, and you get some degree of stretch to your back.
Inversion therapy tables are see-saw like contraptions designed to use gravity to decompress the spine. They have been around for more than twenty years already, so today’s models offer more in terms of comfort and ease of use. But the principle is the same: use a platform balanced on a horizontal rod, with a mechanism to offer some controlled resistance. You lie face up on the platform (more expensive models allow you to be face down), lock your feet into the foot carriage either by hooking your insteps onto rollers, or wearing gravity boots strapped to the carriage; and raise your arms in varying angles to control the amount of tilt. Arms extended straight above your head result in the maximum angle, usually around 45 degrees. The weight of your torso pulls gently on your spine, and you get some degree of stretch to your back.
So is inversion therapy good for your back? Can it relieve lower back pain? The answer is “yes” for some cases of low back pain. I wrote about how low back pain can come from bulging discs, an acute or chronic low back strain, and even abnormal communication between the brain and the postural muscles. Low back stiffness is usually caused by inactivity, carrying too much abdominal weight, which places too much pressure on the small facet joints in the back of the spine; and basically “turned off” muscles; i.e. poorly conditioned, inactive erector spinae and multifidi muscles that surround the spine. This is common in people who sit more than four hours a day on a regular basis and don’t exercise.
Inversion table therapy should be helpful for some cases of disc bulges and back stiffness. Do not do it for an acute lumbar strain. And if your problem is due to miscommunication between the brain and postural muscles, inversion therapy may offer some relief, but the symptoms will quickly return, as this type of back problem originates in the motor neurons of the brain, not the back muscles.
Before you go out and buy one, realize that you must be able to physically handle being inverted. Although you shouldn’t stay inverted for more than 30 seconds or so, for some people, just a few seconds of being inverted (upside down) can be unpleasant, and dangerous. If you have the following conditions, you should not use inversion therapy for back pain:
- metal plates, hardware in spine or lower extremities
- history of migraine headaches
- eye diseases (especially glaucoma)
- history of vertigo, tinnitus, Meniere’s disease
- recent surgery to ankles, knees, hips, spine
- cardiovascular disease; heart problems
- risk factors for stroke
- aortic aneuyism
- osteoporosis
Basically, aside from back pain, you need to be in fairly good physical shape to do inversion therapy; otherwise the risks exceed the benefit. Ask your doctor if it is OK for you to do it.
Now, for those who meet the physical criteria. As in anything new, start slowly. Get used to your machine– how it feels, how responsive it is to your movements. Know how long you can be inverted before you start feeling dizzy. The proper way to do it is to start with small angles first, maintaining the position for a minute or so. Attempt steeper angles, but in small increments. You will find that the steeper you go, the less time you are able to hold the position, due to blood pressure increasing in the head from the effects of gravity. Take your time. Do not attempt a 45 degree incline your first day. You don’t even have to go that far, ever, as long as you can get a good stretch to your low back.
As you get comfortable with your inversion therapy table, you can do some gentle and slow spinal twists as you are inverted. Just rock your upper torso and shoulders from side to side. You may hear some pops as some vertebral facet joints decompress. The popping sound is just air pockets shifting in the joint capsules as the space increases from the stretching.
Lastly, adhere to this tip, which most people forget when doing inversion therapy: concentrate on relaxing your spinal muscles. In fact, before you start your inversion therapy session, close your eyes and take three, deep breaths through your nose, and slowly exhale through your mouth. Focus on your diaphragm expanding, drawing in the air, then relaxing it as you exhale. If you are tensed up, your back muscles will NOT allow the table to decompress your spinal joints. Back muscles are strong and can easily prevent the spine from elongating if they are under contraction. Remember, the goal of inversion therapy is to target the spinal discs and facet joints, not the back muscles themselves. The spine is where most of the symptoms of back pain and stiffness originate.
There are many brands of inversion tables, and varying degrees of quality. The basic ones are rated to about 250 pounds max (person’s weight). The Teeter Power VI Inversion Table with Gravity Lock Ratchet table is a higher-end table that doesn’t require you to raise your arms in order to tilt the table. A motorized inversion table may offer better traction to the lumbar spine, as the act of raising the arms contracts the back muscles which is definitely undesired when attempting to stretch the spine. And if money is not an issue, you may consider the Teeter DFM – Decompression and Functional Movement Table
table is a higher-end table that doesn’t require you to raise your arms in order to tilt the table. A motorized inversion table may offer better traction to the lumbar spine, as the act of raising the arms contracts the back muscles which is definitely undesired when attempting to stretch the spine. And if money is not an issue, you may consider the Teeter DFM – Decompression and Functional Movement Table , a commercial-grade table designed with input from doctors and therapists. This table can be used in the prone (face down) OR supine (face up) position, and offers progressive decompression therapy.
, a commercial-grade table designed with input from doctors and therapists. This table can be used in the prone (face down) OR supine (face up) position, and offers progressive decompression therapy.
My advice is if you are a chronic back pain sufferer, go with a higher end machine because you will be using it a lot. That way, you can rest assured that you’ll be getting a sturdier machine with better construction that will last longer. The cheaper models still can do a decent job, but they are made of weaker material and tend to be more “rickety” as they are held together by bolts and thinner metal tubing.
by Pain Doc | May 17, 2011 | Uncategorized
 I’ve been fielding a lot of questions about bulging discs lately. Here are some of the questions I get:
I’ve been fielding a lot of questions about bulging discs lately. Here are some of the questions I get:
The short answer to the first question is “yes” if the bulge is not severe and the body still has in place the mechanisms to keep the disc living and healthy (see below).

The other answer to the first question is “no” if the disc bulge is the result of breakdown of the nutrient-delivery mechanism to the disc. If this is the case, it is a matter of time before the disc totally degenerates. Physical therapy, chiropractic, spinal decompression and exercises can slow it down, but one cannot do these things indefinitely and often enough to stop the progression.
It’s important to know that your spinal discs are mostly avascular; meaning, don’t have a direct blood supply. Discs get their nutrients (water, oxygen, glucose, minerals, vitamins) via slow absorption from the capillaries directly underneath the vertebral end plates. At the end of the day, your discs flatten from the effects of gravity. As you sleep, they soak up fluids and expand, so that by the time you wake up in the morning you are at least 5 mm taller than when you first went to bed. This is called the diurnal cycle of fluid movement in and out of the disc and is the major means of nutrient delivery.
At the center of the disc is the nucleus, which has tiny cells that make the proteoglycan molecules responsible for attracting and holding onto water. This maintains a hydrostatic pressure that allows the disc to bear about 80% of the weight applied to its spinal level. These cells, similar to chondrocytes that make collagen in the joints, are the most active when the pressure in the disc is about 3 atmospheres. If the pressure is higher (obese individuals, those who carry heavy weight frequently at work) or lower, the cells make less of these molecules, putting the disc at greater risk of drying out. Injuries to the internal part of the disc or vertebral bodies can increase the volume of the nucleus, drastically reducing its hydrostatic pressure and slowing down proteoglycan synthesis. This is one of the pathways of degenerative disc disease, or DDD as the posterior (facet) joints, which are not designed for bearing much weight take on the responsibility of the disc and quickly wear down, forming the familiar osteophytes (bone spurs) seen on X-ray and MRI studies.
Here are the basic risk factors for developing DDD/ bulging discs:
1) History of Structural Damage to the Disc or Vertebra
Single event trauma to the spine resulting in damage to the vertebral end plates . An example would be a parachuter landing hard on the ground on his feet. This can cause a small injury, or even a significant compression fracture to the bony end plates– the surfaces to which the disc attaches. This is bad news, because nutrients to the disc (blood, oxygen, glucose) traverse through these end plates from the top and bottom of the disc. If it is damaged, the area calcifies and “shuts the gate,” depriving the disc of critical nutrients needed to stay healthy. This sets the stage for a slow procession of degeneration over the years which will have phases of back pain, stiffness, disc bulging, stenosis, and in severe cases leg pain, leg weakness and altered sensation.
Repetitive, axial loads to the spine. An axial force is one that travels straight down the spine, while standing. If you are in a job that requires frequent heavy lifting, especially above the shoulders; or requires you to carry 50 or more pounds of gear most of the day, you are placing axial loads on your spine. Similar to #1, it can slowly damage the vertebral end plates and damage the nutrient delivery system to the disc.
2) Hereditary Factors – there are respected studies that strongly suggest a genetic component to DDD. One study showed that there is a 50% greater chance of developing severe disc degeneration in the relatives of past disc surgery patients. Another study found mutations in the genes responsible for the synthesis of proteoglycan molecules, which are responsible for water retention in the disc. If the disc cannot attract and hold onto water, it cannot maintain its hydrostatic pressure. As a result, it loses its ability to distribute weight and slowly dessicates (dries out).
3) Occupation. This is pretty obvious. Those who work with heavy machinery or require heavy lifting are more prone to developing bulging discs.
4) Smoking. Smoking damages the fine blood vessels that the disc depends on to deliver nutrients. It also generates a lot of free radicals, which can damage the disc further. Some surgeons require patients to be “smoke-free” for at least three months prior to surgery.
So, here are the lessons to take here. First, if you have a parent who suffers from bulging discs and degeneration, realize that you have a 50% greater chance of developing them on your own. You may have a mutant gene that is making defective collagen in your disc, making it a ticking time bomb ready to go off in the near future. Your best bet is to minimize the expression of this gene, and a good way to do it is to eat as healthy as you can; ditch the toxins (smoking, excessive alcohol and sugar); avoid getting overweight, and maintain positive thoughts (may affect gene expression to your benefit).
Secondly, avoid unnecessary axial forces to your spine. Stay away from things that involve hard landings on your feet, and don’t lift weights in a way that places pressure to your lower back.
by Pain Doc | Sep 13, 2010 | Low Back Pain
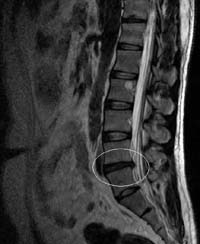
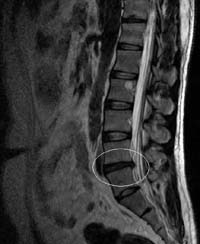
Image via Wikipedia
Lower back pain presents in a range of severity depending on the structures generating the pain.
A simple sprain/strain can still cause extreme pain, swelling, and immobilization for a couple of days but should completely resolve after a few weeks with proper care and rest. Lumbar sprain/strains are associated with lifting something heavy, or even simply bending or twisting at the waist; weight lifting, sports injuries and trauma like a car accident. By definition, they are limited to injury to the muscles, fascia, tendons and ligaments. The pain is limited to the area of injury.
A lumbar disc bulge occurs when a disc “bulges” outwards due to weakness or injury. A disc is a tough, fibrous ligament that holds the lumbar vertebrae together at the vertebral body. The disc’s outer periphery, called the annulus, resembles a slice of an onion, with multiple rings of fibrous tissue encasing a jelly-like material called the nucleus pulposus. While tough and strong, it allows movement of the individual vertebrae.
By definition, a disc bulge is still intact and has not ruptured (as opposed to a disc herniation or rupture). The bulge represents a weakened area in the annulus that allows the nucleus to gravitate towards a section of the periphery, usually the posterior (rear-facing) edge, facing the spinal canal (where nerve tissue is present). It can be a broad-based bulge, or a more focal bulge. If it is greater than 5mm (measured from the edge of the vertebral body to the tip of the bulge) it is clinically significant. Many people have disc bulges and have no back pain at all; in fact, it is normal for the discs to bulge slightly in the weight bearing position (standing).
The problem occurs when the bulge contacts nerve structures. If large enough, they can contact the thecal sac (contains the spinal cord and cauda equina) by bulging backwards into the canal, and they can press on spinal nerve roots by bulging to the sides. The spinal nerve roots branch out in pairs from either side and exit holes formed between adjacent vertebrae called vertebral foramen, or lateral canals. A disc bulging to the posterior and side can narrow this opening and pinch the nerve root causing pain to travel down the buttock or leg, depending on which nerve root.
TREATMENT:
If your lower back pain is felt deep, and you can make it hurt more by bending your lower back backwards and to the side, you may have a disc bulge. You may or may not have pain and/or numbness going down the buttock and leg (same side of the pain). If it happened while lifting something heavy, the diagnosis is more likely. If you have extreme, unchanging pain with more constant leg pain or paresthesias (numbness, tingling) that does not get better with ice and rest, you may have a disc rupture (also called prolapse) where the inner nucleus had broken through the annulus and is in the spinal canal or lateral canal. If you have changes in your gait (walk) such as foot drop, weakness in your legs, difficulty walking upstairs, then the diagnosis of disc prolapse is more probable.
Disc bulges can be managed with conservative treatment like home care, chiropractic, and physical therapy. Disc prolapses should be evaluated by an orthopedic surgeon or neurosurgeon. An MRI should be ordered to evaluate the extent of the injury.
If you suspect you have a disc bulge, take care not to aggravate it. No heavy lifting, no jumping activities (basketball, badminton– anything where your feet leave the floor and land hard).
Discs usually bulge backwards (posterior), so do movements that encourage the bulge to move back to center. Lie on your back and bring both knees to your chest (ok to use your arms to grab your knees while they are bent, and pull and hold to your chest). This will put your lumbar spine in flexion, or a nice convex curl. Your back contour should be like that of an egg, and you should be able to rock back and forth. Maintain the pull, stretching your lower back into this curve. Hold for 30 seconds, then slowly extend your legs on the floor and rest for 15 seconds (optional: put a frozen ice gel pack covered with a kitchen towlette under your lower back during this exercise). Repeat six times. This will have the effect of creating separation between the posterior ends of the lumbar vertebrae, helping to reduce the bulge.
Next, stand and place your hands on your hips, and slowly arch your back backwards, putting your lumbar spine into extension— the opposite curvature as the previous exercise. Bend back until you can’t anymore, but don’t over do it. Hold this position for six seconds, then return to neutral. Repeat eight times. This will have the effect of bringing the posterior ends of the lumbar vertebrae closer together and pushing the nucleus back towards the center.
Do the above series of exercises three-four times a day for a week until the discomfort is gone. At this point, you should focus on doing things to strengthen the disc. Eating a wholesome, healthy diet with enough protein, fat and plant material will help; avoiding destructive activities like smoking, alcohol, and staying up late will enable optimum conditions for tissue healing. Gradually start doing exercises that improve lower back muscle conditioning and coordination.
Getting a series of 6-8 chiropractic adjustments to the lumbar spine may also be helpful in reducing your bulging disc.

 PosturePump Disc Rehydrator
PosturePump Disc Rehydrator Anti-Shock Specialty Shoes
Anti-Shock Specialty Shoes Vari-Desk Height Adjustable Portable Desk
Vari-Desk Height Adjustable Portable Desk


 I’ve been fielding a lot of questions about bulging discs lately. Here are some of the questions I get:
I’ve been fielding a lot of questions about bulging discs lately. Here are some of the questions I get: